Cervical Laminoplasty
What is Cervical Laminoplasty?
Cervical laminoplasty is a surgical technique that removex pressure from the spinal cord in then neck. Pressure on the spinal cord can be due to various causes including degenerative changes, arthritis, bone spurs, disc herniations, OPLL, tumors, or fractures. Frequently this spinal cord pressure, called spinal stenosis, can occur at multiple levels of the cervical spine at the same time. If this pressure is severe enough, symptoms called myelopathy can develop. Laminoplasty may be an excellent option to remove the pressure, allow the spinal cord to heal, and reverse the symptoms.
Who needs Cervical Laminoplasty?
Patients with spinal cord compression and myelopathy would likely benefit from evaluation by a NASS physician. Patients with myelopathy can have various symptoms including numbness, pain, or weakness in the arms or hands, difficulty using their hands, and balance problems. Occasionally, myelopathy can progress to a point where patients have extreme difficulty walking or using their hand for everyday tasks. A NASS physician can perform a thorough history to evaluate your symptoms and any recent changes. A full physical examination including neurologic exam would then be performed. Together, the history and physical provide your NASS physician important information regarding the severity of your spinal disease. Your NASS physician may also order specialized tests such as X-rays, which show the bones of the spine, or an MRI scan, which shows the soft structures in the spine such as the discs or spinal cord. The MRI scan can provide very detailed information regarding the amount of compression on the nerves or spinal cord [Figure 1]. If there is compression on the spinal cord and the patient has symptoms, the NASS physician may suggest surgery to prevent further damage to the spinal cord. Fortunately, spinal cord compression and myelopathy can be treated by taking the pressure off of the spinal cord via surgery."
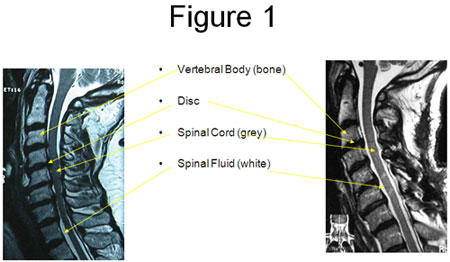
Figure 1. A) A side-view MRI scan showing the cervical spine in a patient with spinal stenosis. Notice the grey spinal cord traveling down from the brain in the spinal canal. There are multiple areas of spinal cord compression which can be seen by loss of the white spinal fluid. B) A side-view MRI scan following a laminoplasty in the same patient. Notice that the white spinal fluid now surrounds the spinal cord throughout the image.
How is Cervical Laminoplasty Performed?
One option for removing compression from multiple levels in the neck is called a cervical laminoplasty. A laminoplasty is performed via an incision in the back of the neck which is called a posterior approach. During surgery, the patient will be lying face down on the operating table. Frequently, specialized monitoring devices are used to check the spinal cord during the surgery to ensure that there is no damage to the spinal cord during the surgery. Instead of removing the bone and other compressive structures, the bone overlying the spinal cord (the “lamina”) is partially cut on both the right and left sides. This creates a hinge on one side of the lamina and a small opening on the other side. The lamina is then moved into the “open” position by elevating the lamina on the open side [Figure 2]. This vastly increases the space available for the spinal cord and takes the pressure off of it. The spinal cord can move away from whatever was compressing it including disc herniations or bone spurs (as seen in Figure 1), and the spinal fluid can then flow around the spinal cord more normally (the white substance seen Figure 1). A spacer made out of bone, metal, or plastic, is usually inserted to hold the spinal canal open [Figure 2]. The final position resembles an open door being help open with a door stop, and many surgeons refer to this technique as an “open-door” laminoplasty. Another type of laminoplasty called a “French-door” laminoplasty is performed by creating hinges on both side of the lamina and an opening in the center of the lamina. The lamina is then opened by elevating both sides and ultimately resembles a French-style patio door.
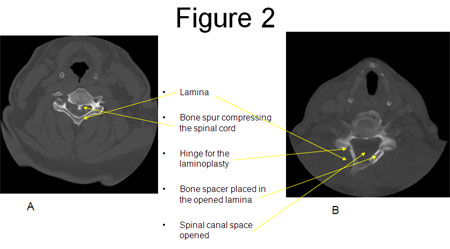
Figure 2. A) Pre-operative CT myelogram showing severe spinal cord compression due to congenital spinal stenosis and a large bone spur. B) Post-operative CT scan showing the neck bone (vertebra) including the lamina. An open-door laminoplasty has been performed. Notice the bone graft that has been placed on the opened side to hold the “door” open.
This procedure, first invented by Japanese surgeons, has been used for over 35 years with excellent results and low rates of complications. Surgery can be performed quite quickly and a fusion is usually not required. Because a fusion is not required, most patients do not notice a significant loss of motion [Figure 3] although some studies have shown that patients have stiffness post-operatively. Both open-door laminoplasty and French-door laminoplasty have similar outcomes.

A

B
Figure 3. A) Post-operative lateral x-ray of the cervical spine showing extension of the spine following a cervical laminoplasty. B) Post-operative lateral x-rays of the same patient showing flexion. Note that the range of motion is maintained after the laminoplasty and that no fusion was performed.
What can I expect?
The main complaint after this kind of surgery is pain in the back of the neck. This pain can be quite severe for several days after surgery, and it then gradually improves over several months. Occasionally, one of the nerves in the neck can be stunned after surgery because of the movement that occurs when the nerve moves back to its normal location after removal of the compression. This nerve “stunning” is called a nerve palsy. This palsy can cause significant weakness, especially in the shoulder, and pain in same region. Fortunately, this palsy is almost always temporary and gets better without any treatment. Overall, the results for a laminoplasty are very good, the surgery is very well tolerated, and serious complications are very rare.
After surgery, patients usually remain in the hospital for 2 – 3 days. A neck collar is used for several weeks after surgery and can be removed when your NASS surgeon approves. Physical therapy may be prescribed by your NASS physician to strengthen the neck muscles after surgery.
Patients who undergo laminoplasty frequently have multiple levels of severe spinal cord compression leading to nerve problems possibly including pain in the arms, numbness, difficulty using their hands normally, and balance problems. These problems can be very debilitating prior to surgery, but fortunately laminoplasty provides excellent decompression of the injured spinal cord. After a laminoplasty, most patients have significant recovery of the nerve function within several months after surgery, if not sooner. This nerve function improves over the next 6 – 18 months as the spinal cord continues to heal itself. Many patients can have complete resolution of the pre-operative symptoms, although long-standing spinal cord compression can lead to permanent nerve damage that never fully recovers.
Various conditions, including those as common as degenerative disc disease, can cause compression on the spinal cord in the neck. This compression can lead to impaired spinal cord function, called myelopathy. Treatment of myelopathy involves removal of the compression from the spinal cord via surgery. Laminoplasty is one of the options available, and it provides an excellent option for treating even severe cases of spinal cord compression. If you think you may have any of these conditions, please see your NASS physician for evaluation.
